A new type of cell could change the focus of CF research
The new cells called ‘ionocytes’ contain the highest number of CFTR proteins compared to other cells in the lungs and were found by two separate groups of researchers, both based in Massachusetts, USA. The researchers also identified a chemical that regulates how much CFTR is produced in these ionocytes.
Why we should care about the discovery of ionocytes?
1. CFTR’s hiding place has been found
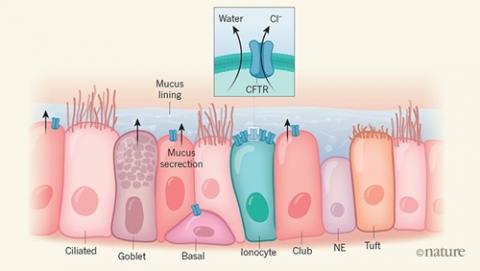
When the researchers looked in detail at the genetic readout of these new ionocytes they found a high readout for CFTR, the mutated gene that causes cystic fibrosis. Comparing the genetic readouts for ionocytes with the other already-known cell types in the lungs, they found that ionocytes make more CFTR than any other cell type.
Before this research came out, previous studies had found that CFTR production in the lungs was complex, with different cell types involved in different places in the lungs. It’s very early days, but the discovery of ionocytes will bring a new, sharper focus to many avenues of CF research.
2. The production control for CFTR has been found
Both studies also found that, as well as containing more CFTR protein than other cells that line the lungs, ionocytes contain a chemical that controls the amount of protein produced.
What does this mean for future CF research?
Although these results are an exciting step forward in CF research, there is much work still to be done to understand just how important it might be. We need to understand more about how ionoctyes work, how CFTR contributes to how they work, and how this goes wrong in cystic fibrosis. In terms of developing new treatments, we need to know how to correct any changes found in ionocytes – either by changing them genetically or by changing them with drugs.
But how does the discovery of ionocytes fit in with what we already know about the cells in the lungs?
What do we already know about lung cells?
We know that there are at least five different types of cell that line our lungs. They all sit snugly next to each other, but do different jobs. These include cells that produce mucus, cells that are responsible for clearing mucus and foreign bodies from the lungs, immune cells that protect against infections, and cells that facilitate the transfer of gases to the blood.
How do we know that they’re there?
One way to tell what type of cells are present in the lining of the lungs is to look at the unique chemical markers that they carry. Imagine these markers as the flag-bearing athletes at the opening ceremony at the Olympics – each athlete carries a flag unique to their country.
Detection of genetic readout is the new kid on the block
Traditionally, researchers used these flags to detect which cells were present in their lab studies. In recent years however, a new way of detecting the presence of different lung cells has emerged: looking at genetic read outs of which proteins each cell type is making.
Our DNA is the blueprint of our cells, and every cell has the same blueprint. However, different cells will read different parts of this blueprint depending on the job that they’re going to do (in the same way that you wouldn’t try and make all the recipes in a cookery book in one go, cells read the instructions for making a protein one recipe at a time!). This new kind of analysis can detect which instruction the cells are reading – they do this by analysing the cells’ RNA, a messenger in the cell that converts genes protein.
Why haven’t genetic readouts always been used to detect cell types?
This way of measuring the cell’s genetic readout has been available for some time, but without the technology to be so precise. Recently, however, technology has made it feasible to study genetic readouts in individual cells, using far less material (or RNA) than previously. Before these advances the amount of RNA from one cell wasn’t enough to get an accurate readout.
Different technology has meant that researchers can cleanly separate one cell type from another. If the cells weren’t properly separated, the readout from one cell may have been ‘contaminated’ with the readout from the neighbouring cell, giving misleading results. Much more research still needs to be done to understand the true significance of these findings for future CF treatments, but their discovery marks a milestone in CF research.
To read more about this research, you can read a piece in the Nature science journal on these two research papers. The research papers, by Daniel Montoro and colleagues based in Massachusetts General Hospital, Boston USA and by Lindsey Plasschaert and colleagues based at Novartis, Massachusetts are also available online.
